April 25, 2025
Finding Relief: The Complete Guide to Colitis Medications
If you’re navigating the sometimes overwhelming world of colitis medication, you’re not alone. Nearly a million Americans with ulcerative colitis are walking this same path alongside you, searching for relief and healing.
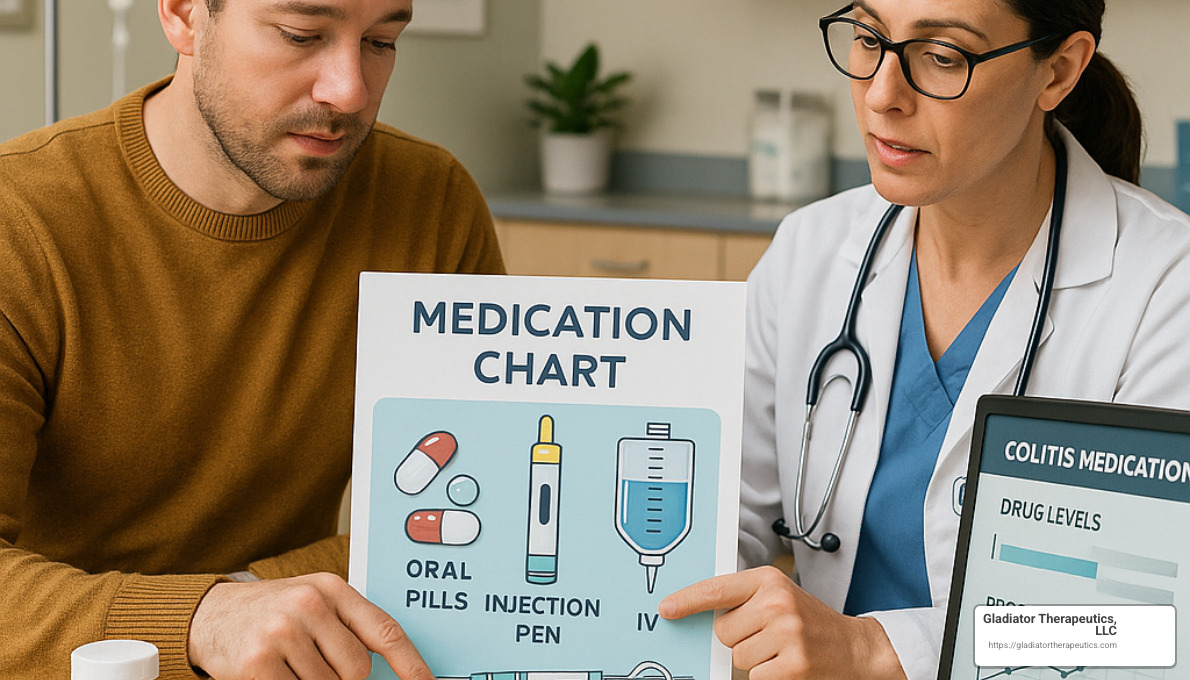
Here’s a quick overview of the main treatment options your doctor might discuss with you:
| Medication Class | Examples | Used For | How Administered |
|---|---|---|---|
| Aminosalicylates (5-ASAs) | Mesalamine, Sulfasalazine | Mild to moderate cases | Oral, rectal (enema/suppository) |
| Corticosteroids | Prednisone, Budesonide | Moderate to severe flares | Oral, rectal, IV |
| Immunomodulators | Azathioprine, Methotrexate | Long-term maintenance | Oral, injection |
| Biologics | Infliximab, Adalimumab | Moderate to severe cases | Infusion, injection |
| Small Molecules | Tofacitinib, Ozanimod | When other treatments fail | Oral |
Living with colitis means more than just managing symptoms – it’s about finding a path to healing your intestinal lining and preventing future complications. Colitis medication is the cornerstone of this healing journey, offering hope and relief when inflammation threatens your wellbeing.
I remember talking with Sarah, a patient who described her first successful treatment as “like someone finally turning down the volume on a blaring radio that had been playing for years.” That’s the power of finding the right medication approach – it can transform your daily experience.
Today’s treatment options offer more promise than ever before. We’ve moved beyond the one-size-fits-all approaches of the past into an era of personalized medicine custom to your specific type of colitis, its severity, and your individual health needs.
Whether you’ve just received your diagnosis or you’re exploring new options after years of treatment, understanding your medication choices empowers you to participate actively in your care. Your goal – and your healthcare team’s goal – is beautifully simple: reduce inflammation, relieve those difficult symptoms, prevent future flares, and help you reclaim your quality of life.
Finding your perfect medication match might take some trial and error. Be patient with the process. Many people need to try different combinations before finding what works best for their unique situation. This is a marathon, not a sprint – and with each step, you’re moving closer to better health.

What Is Colitis? Types, Symptoms & Why Meds Matter
Imagine your digestive system as a well-orchestrated symphony. When colitis enters the picture, that harmony is disrupted by inflammation in your colon (large intestine). But “colitis” isn’t just one condition – it’s actually a family of related digestive disorders, each with its own personality.
Ulcerative colitis starts in the rectum and can spread upward through your colon like watercolor on paper – in one continuous area. The inflammation attacks the innermost lining, creating painful ulcers that can bleed during bowel movements.
Crohn’s disease, while not exclusively a colitis (it can appear anywhere from mouth to anus), frequently involves the colon. Unlike its ulcerative cousin, Crohn’s inflammation appears in patches – like islands of inflammation with normal tissue in between – and digs deeper, affecting all layers of your intestinal wall.
Then there’s microscopic colitis, the stealthy variant that’s invisible to the naked eye during a colonoscopy. As the name suggests, it can only be confirmed when tissue samples are examined under a microscope, yet it causes persistent watery diarrhea that significantly impacts quality of life.
What binds these conditions together? A case of mistaken identity. Your immune system, designed to protect you, somehow gets its wires crossed and attacks your own digestive tract. This immune dysregulation leads to chronic inflammation, tissue damage, and the roller-coaster of symptoms that make living with colitis so challenging.
Most forms of colitis follow an unpredictable pattern of flare-ups and remission periods. That’s precisely why colitis medication plays such a crucial role – both to calm the inflammation during active flares and to maintain peace during periods of remission.
Without proper treatment, the ongoing inflammation can lead to serious complications beyond daily discomfort – from severe blood loss and anemia to malnutrition, increased cancer risk, dangerous colon widening (toxic megacolon), intestinal perforation, and eventually, surgical intervention.
For a deeper dive into what triggers these conditions, visit our comprehensive guide on causes of colitis.
Recognizing Early Warning Signs
Catching colitis symptoms early can make all the difference in treatment success. Your body will typically send several distress signals that shouldn’t be ignored:
Bloody diarrhea often serves as the most recognizable red flag. This can range from slight streaks of blood to predominantly bloody stools that understandably cause concern. Alongside this, abdominal pain and cramping create discomfort that might temporarily ease after a bowel movement – only to return later.
The constant urgency and tenesmus – that frustrating sensation of needing to rush to the bathroom, only to feel like you haven’t completely emptied your bowels – can make simple activities like shopping or commuting anxiety-inducing experiences.
Fatigue with colitis isn’t your ordinary tiredness. It’s often profound exhaustion that doesn’t improve with rest, partly due to the inflammatory response and potential anemia from blood loss. Many patients describe it as feeling “wiped out” regardless of how much they sleep.
Weight loss happens unintentionally as appetite diminishes and nutrient absorption becomes compromised. During severe flares, fever might develop, and overall reduced appetite further compounds nutritional challenges.
The severity of these symptoms typically mirrors the extent of inflammation. Mild cases might involve just a few loose stools daily with occasional cramping, while severe flares can mean 10+ bloody bowel movements daily, debilitating pain, and systemic symptoms that make normal life impossible.
Recognizing these warning signs early allows for faster intervention with appropriate colitis medication, potentially preventing a mild irritation from becoming a full-blown crisis. For a comprehensive symptom checklist, visit our detailed guide on recognizing colitis symptoms.
Colitis Medication 101: Main Drug Classes Explained
Diving into colitis medication can feel like learning a new language. With so many options and complicated names, it’s easy to feel overwhelmed. Let’s break down these medications into simple terms so you can better understand what your doctor might recommend.
Aminosalicylates (5-ASA) at a Glance
Think of aminosalicylates as the gentle first responders for colitis. They’re typically the first treatment doctors reach for when dealing with mild to moderate ulcerative colitis. These medications work right where they’re needed – inside your intestines – to calm inflammation.
Mesalamine (found in brands like Asacol HD, Lialda, and Pentasa) is the most commonly prescribed 5-ASA. It works by blocking certain chemicals in your intestinal lining that trigger inflammation. Other options include sulfasalazine, which combines 5-ASA with a sulfa antibiotic, though it tends to cause more side effects than newer options.
What makes these medications versatile is how they can be delivered. You might take them as pills that release medicine at different points in your digestive system, or as suppositories or enemas that target specific areas of inflammation. Most people tolerate 5-ASAs quite well, with only mild side effects like headaches or occasional nausea.
As Dr. Maria Chen, a gastroenterologist, puts it: “5-ASAs are the workhorses of ulcerative colitis treatment. They’re effective for many patients with mild to moderate disease and have an excellent safety profile, making them suitable for long-term use.”
Corticosteroids: Quick Relief, Not Forever
When colitis flares up severely, corticosteroids often come to the rescue. These powerful anti-inflammatory medications work quickly to calm an angry colon. Think of them as the fire extinguisher in your medicine cabinet – great for emergencies, but not something you want to use every day.
Prednisone is the most well-known steroid for colitis. It works by suppressing multiple inflammatory pathways throughout your body. While this provides fast relief, it also explains why steroids cause so many side effects – they affect your entire body, not just your colon.
A newer steroid called budesonide (found in Entocort EC and Uceris) works more locally in the intestines with fewer body-wide effects, making it a gentler option for some patients.
One unique aspect of steroid treatment is the “taper” – you can’t just stop taking them suddenly. Your doctor will create a schedule to gradually reduce your dose over weeks or months. This gives your body time to resume its natural cortisol production.
“Steroids are like firefighters,” explains Dr. James Wilson, an IBD specialist. “They’re excellent at putting out the fire of a flare-up, but you wouldn’t want firefighters living in your house permanently. Similarly, we don’t want patients on steroids long-term due to their side effect profile.”
Those side effects can be significant – weight gain, mood swings, sleep problems, increased blood sugar, bone loss, and higher infection risk. This is why steroids are for short-term use only.
Immunomodulators for Long-Term Control
When 5-ASAs aren’t enough or you find yourself needing steroids too often, immunomodulators might be the next step. These medications help maintain control of your colitis over the long haul.
Azathioprine (Imuran) and 6-mercaptopurine (Purinethol) are the most commonly used immunomodulators for colitis. They work by broadly dampening your immune response, which reduces the inflammation attacking your intestines. Unlike steroids, they work slowly – often taking 3-6 months to reach full effectiveness – but can provide stable, long-term control without steroid side effects.
Methotrexate is another option, originally developed as a cancer treatment but used at much lower doses for inflammatory conditions. For very severe cases that land you in the hospital, your doctor might suggest cyclosporine or tacrolimus as “rescue” therapies.
These medications require regular blood tests to monitor for potential effects on your bone marrow and liver. While this might sound intimidating, most side effects are manageable and reversible if caught early. Your doctor will keep a close eye on your blood counts, liver function, and overall health while you’re taking these medications.
“Immunomodulators have been a mainstay of IBD treatment for decades,” notes Dr. Sarah Ahmed, an IBD researcher. “While newer biologics get more attention, these medications remain valuable tools, especially in combination therapy approaches.”
Biologics & Biosimilars: Targeted Immune Blockers
Biologics represent one of the biggest breakthroughs in colitis medication over the past two decades. Unlike traditional medications made through chemical processes, biologics are created from living cells and precisely target specific parts of the immune system.
Think of biologics as smart missiles rather than carpet bombs – they zero in on particular inflammatory proteins like TNF-alpha, integrins, or interleukins. By blocking these specific inflammatory pathways, they can effectively turn down the volume on intestinal inflammation without broadly suppressing your entire immune system.
The most established biologics are anti-TNF agents like infliximab and adalimumab. They block a protein called tumor necrosis factor (TNF) that drives inflammation. Vedolizumab works differently, targeting only gut inflammation by preventing inflammatory cells from traveling to your intestines. The newest class includes ustekinumab and other medications that block interleukins, another family of inflammatory proteins.
You might also hear about “biosimilars” – these are highly similar versions of original biologics that become available after patents expire. They undergo rigorous testing to ensure they work just as well as the originals, often at a lower cost.
Biologics are typically given either through an IV infusion at a medical facility every few weeks, or as self-administered injections at home. While powerful, they do carry some risks, including increased infection susceptibility and infusion reactions. Your doctor will test you for tuberculosis and hepatitis before starting these medications.
For the latest research on biologic therapies, you can explore information from the Crohn’s and Colitis Congress.
Targeted Synthetic Small Molecules
The newest kids on the colitis treatment block are small molecule drugs. Unlike biologics, which are large, complex proteins, these are smaller, synthetic compounds that can be taken as pills rather than injections.
JAK inhibitors like tofacitinib (Xeljanz) and upadacitinib (Rinvoq) block enzymes called Janus kinases that play a key role in inflammation. By interrupting these signaling pathways, they can effectively reduce intestinal inflammation.
Another exciting class is S1P receptor modulators like ozanimod (Zeposia) and etrasimod. These work by essentially trapping inflammatory cells in your lymph nodes, preventing them from traveling to your intestines to cause damage.
The convenience of taking a pill instead of getting an injection or infusion is a big advantage for many patients. These medications also don’t trigger antibody formation (which can sometimes happen with biologics), and they clear from your body more quickly if you need to stop treatment.
However, being newer means we have less long-term safety data. JAK inhibitors carry warnings about increased risks of serious infections, blood clots, and certain cancers. Your doctor will help weigh these potential risks against the benefits for your specific situation.
“Small molecules represent an exciting frontier in IBD treatment,” explains Dr. Robert Lee, a pharmaceutical researcher. “Their oral administration and targeted mechanism offer advantages for many patients, though we’re still learning about their long-term safety profiles.”
Choosing the Right Colitis Medication for You
Finding the right colitis medication isn’t one-size-fits-all – it’s more like finding a custom suit that fits your specific condition and life circumstances. Your doctor will consider several important factors when recommending treatment.
First, how severe is your colitis? Mild cases might respond well to 5-ASAs alone, while moderate to severe disease often requires stronger medications like immunomodulators or biologics. The location of your inflammation matters too – rectal inflammation might be treatable with suppositories, while widespread colitis usually needs oral or injectable medications that can reach throughout your colon.
Your personal factors play a huge role too. Your age, other health conditions, pregnancy plans, and even your lifestyle preferences (like whether you’re comfortable with injections) all influence which medication might work best for you. Previous medication experiences also provide valuable clues – if one type of medication didn’t help or caused side effects, that narrows the field.
Some patients prioritize effectiveness above all else and are willing to accept higher risks of side effects. Others prefer more conservative approaches. Having an honest conversation with your doctor about your priorities helps ensure you find a treatment that aligns with your values.
Dr. Elena Martinez, an IBD Center Director, emphasizes: “There’s no one-size-fits-all approach to colitis treatment. The right medication regimen is one that effectively controls inflammation while aligning with the patient’s values, lifestyle, and risk tolerance.”
Side Effects to Watch With Colitis Medication
While colitis medications can be life-changing, being informed about potential side effects helps you partner with your doctor to use them safely.
Most colitis medications affect your immune system to some degree, which can increase your infection risk. Pay attention to symptoms like fever, persistent cough, or unusual infections, and stay current with recommended vaccinations. Some patients find it helpful to take extra precautions during cold and flu season.
Regular lab monitoring is an important part of colitis treatment. Blood tests help catch potential issues before they become serious problems. Your doctor will check your blood counts to ensure your bone marrow is functioning well, monitor your liver and kidney function, and sometimes measure drug levels to ensure you’re getting the right amount of medication.
Bone health deserves special attention, particularly if you take corticosteroids. These medications can significantly increase your risk of osteoporosis. Your doctor might recommend calcium and vitamin D supplements, bone density screening, and weight-bearing exercise to protect your bones.
Some medications can affect your skin, causing increased sun sensitivity or rashes. With long-term immunosuppression, there’s also a small increased risk of skin cancers, so regular skin checks become important.
Other side effects might include headaches (common with 5-ASAs), stomach upset, fatigue, or hair thinning with certain medications. The good news is that most side effects are either preventable, manageable, or reversible.
“The key to managing medication side effects is awareness and proactive monitoring,” advises Dr. Rachel Kim, a pharmacist specializing in IBD. “By staying in close communication with your healthcare team, most side effects can be addressed before they become serious problems.”
Personalizing Your Treatment Plan & Monitoring Progress
Finding the right approach to manage colitis isn’t about following a cookie-cutter plan—it’s about creating a strategy that fits your unique needs, lifestyle, and response to treatment.
At the heart of effective colitis management is shared decision-making between you and your healthcare team. This isn’t just medical jargon—it’s about having real conversations where your voice matters. When you meet with your doctor, come prepared to discuss what matters most to you: Is it getting back to work? Being able to travel? Reducing urgent bathroom trips? These priorities help shape treatment decisions that align with your goals.
“The most successful treatment plans I’ve seen are those where patients are active participants, not passive recipients,” says Dr. Thomas Wong, gastroenterologist. “When patients understand their options and voice their concerns, we make better decisions together.”
Today’s approach to colitis medication goes beyond just prescribing pills and hoping for the best. Modern treatment includes sophisticated monitoring to ensure your medications are working optimally. One game-changing approach is therapeutic drug monitoring—measuring the actual levels of biologics and certain immunomodulators in your bloodstream. This isn’t just extra testing; it helps your doctor understand why a medication might be losing effectiveness or causing side effects, and guides precise dose adjustments.
Regular assessment doesn’t stop with blood tests. Your doctor will likely track your progress through:
- Symptom tracking (either through diaries or apps)
- Quality of life questionnaires that capture how you’re really feeling
- Biomarkers like fecal calprotectin that show inflammation levels without invasive procedures
- Periodic colonoscopies to directly visualize healing
“We’re moving away from treating solely based on symptoms,” explains Dr. Wong. “The goal now is to achieve not just symptomatic improvement but also endoscopic healing—actually resolving the inflammation visible during colonoscopy. This deeper level of healing is associated with better long-term outcomes.”
Think of it like fixing a leaky roof—you don’t just want to stop seeing water dripping (symptoms); you want to repair the actual hole (inflammation) to prevent long-term damage.
For those whose colitis has autoimmune components, additional considerations may apply. You can find more specialized guidance on our autoimmune disease management page.
Administration Routes & Dosing Hacks
Taking colitis medication correctly makes a huge difference in how well it works. Let’s look at practical tips for each type of medication delivery.
If you take oral medications, timing can be everything. Some tablets need to be taken with food to prevent stomach upset, while others work best on an empty stomach. Delayed-release formulations must be swallowed whole—crushing or chewing them defeats their special coating designed to release medication in specific parts of your digestive tract. If you’re juggling multiple medications, a simple pill organizer can be a lifesaver, especially during busy mornings or when traveling.
For those using rectal treatments, the experience can initially feel awkward or uncomfortable, but a few tricks can help. “One practical tip I share with patients starting rectal therapies is to use them just before bedtime and lie on your left side for a few minutes afterward,” suggests Maria Lopez, IBD nurse specialist. “This simple positioning trick helps the medication distribute more effectively in the colon.” Suppositories typically reach about 10 cm into the rectum, while enemas can reach higher into the colon—up to the splenic flexure (the bend near your spleen). Many people find foam preparations easier to retain than liquid enemas.
Self-injections might seem intimidating at first, but modern pre-filled pens have made the process much simpler. Letting your medication warm to room temperature (usually 30 minutes out of the refrigerator) makes injections more comfortable. Remember to rotate injection sites to prevent tissue damage—many medications come with tracking sheets to help you keep track of where you last injected.
For those receiving infusions of biologics, planning can make infusion days smoother. Infusions take place at specialized centers or sometimes at home with a visiting nurse. Sessions can last anywhere from 30 minutes to several hours, so bringing entertainment like books, podcasts, or meditation guides helps pass the time. Some people experience fatigue afterward, so consider scheduling infusions when you can rest afterward if needed.
When Medication Isn’t Enough: Considering Surgery
Despite our best efforts with colitis medication, sometimes surgery becomes the most sensible next step. This isn’t a failure—it’s simply another treatment option that might offer the best quality of life. About 30% of people with ulcerative colitis will eventually need surgery, while the lifetime surgery risk for Crohn’s disease is even higher at 70-80%.
Surgery becomes worth considering when medications aren’t providing adequate relief, side effects become intolerable, or complications develop. Sometimes, precancerous changes detected during surveillance colonoscopies make surgery the safest choice. For children with inflammatory bowel disease, persistent growth issues despite optimal therapy might tip the scales toward surgical intervention.
For ulcerative colitis, surgical options have advanced significantly. Total proctocolectomy with ileostomy involves removing the entire colon and rectum, then bringing the end of the small intestine through the abdominal wall to form a stoma where waste collects in an external pouch. While this sounds dramatic, many people find tremendous relief from symptoms and enjoy an active lifestyle after adapting to life with an ostomy.
Another option is the J-pouch procedure (ileal pouch-anal anastomosis), where after removing the colon and rectum, surgeons create an internal pouch from the small intestine and connect it to the anus. This preserves a more conventional bathroom experience without an external bag, though bowel movements are typically more frequent than before.
“Surgery is not a failure of medical therapy—it’s another treatment option that can provide excellent quality of life,” emphasizes Dr. Sarah Johnson, colorectal surgeon. “Many patients wish they hadn’t delayed surgery once they experience life without constant symptoms.”
Even after surgery, some patients—particularly those with Crohn’s disease—may need maintenance medications to prevent recurrence. The journey doesn’t necessarily end with surgery, but for many, it opens a new chapter with significantly improved quality of life.
Lifestyle, Diet & Flare Management While on Meds
Living with colitis goes beyond just taking your medications. The everyday choices you make about food, stress, and activity can significantly impact how well your colitis medication works and how you feel overall.
When Sarah was first diagnosed with ulcerative colitis, she thought medications alone would solve everything. “I quickly learned that what I ate, how I managed stress, and even how much I slept played huge roles in how I felt,” she shares. “The medications created the foundation, but my daily habits built the house.”
Your diet can either support or undermine your treatment plan. Many people find keeping a food journal helps identify personal trigger foods that worsen symptoms. Common culprits include high-fiber foods during flares, dairy products (especially if you’re lactose intolerant), spicy dishes, alcohol, caffeine, and carbonated drinks. But everyone’s triggers are different – what bothers your friend with colitis might be perfectly fine for you.
Working with a dietitian who specializes in IBD can be incredibly helpful. They can guide you through elimination diets safely and ensure you’re getting proper nutrition even when your diet is restricted. This is particularly important since colitis can increase your risk of deficiencies in iron, B12, vitamin D, and other nutrients.
Stress management isn’t just a nice-to-have – it’s essential. “The gut-brain connection is real,” explains Dr. Lisa Morgan, gastroenterologist. “Many patients can literally feel their intestines react during stressful situations.” Finding effective ways to manage stress can help extend your periods of remission and make your medications more effective.
Mindfulness meditation, yoga, deep breathing exercises, and even regular walks in nature can all help tame the stress response. Many patients find cognitive behavioral therapy particularly helpful for developing coping strategies specific to the challenges of living with a chronic condition.
Don’t underestimate the power of good sleep. Research shows poor sleep quality correlates with increased inflammation and higher risk of flares. Establishing a consistent sleep schedule, creating a cool, dark sleeping environment, and addressing symptoms that might wake you (like nighttime bathroom trips) can all improve your overall health.
Regular exercise offers multiple benefits for colitis patients. Beyond the obvious stress reduction, physical activity helps maintain bone density (particularly important if you’re taking steroids), improves immune function, boosts mood, and may even have direct anti-inflammatory effects. Start gently, especially during flares, with low-impact activities like swimming, walking, or yoga.
Many patients wonder about supplements. While they shouldn’t replace prescribed medications, certain supplements may complement your treatment. Vitamin D supplementation is often recommended as deficiency is common in IBD and may contribute to inflammation. Probiotics show promise for some patients, though research suggests specific strains matter – VSL#3 and Mutaflor have the strongest evidence for ulcerative colitis.
“I’ve found that balancing my medications with lifestyle approaches gives me the best control,” says Michael, who’s managed Crohn’s colitis for a decade. “When I’m exercising regularly, eating carefully, and keeping my stress in check, I need less rescue medication and have longer stretches without symptoms.”
For comprehensive strategies that go beyond medications, check out our detailed guide on strategies for colitis recovery.
Handling a Flare or Side Effect Fast
Even with the best management plan, flares happen. Having a clear action plan can help you respond quickly and effectively when symptoms worsen.
The most important rule: don’t wait too long to seek help. Many patients try to “tough it out,” hoping symptoms will improve on their own. This often leads to more severe flares that are harder to control. Contact your gastroenterologist at the first sign of worsening symptoms – increasing bowel frequency, blood in stool, new abdominal pain, or extreme fatigue.
“I tell all my patients to have a flare plan in writing,” says IBD nurse coordinator Jamie Wilson. “When you’re feeling awful, you don’t want to be figuring out what to do. You want clear steps to follow.”
Your flare plan might include temporarily adding rectal therapies if your symptoms are focused in the lower colon, a short course of steroids, or adjusting your existing medication doses. Never stop your current medications unless specifically directed by your healthcare provider – this can sometimes make things worse.
During a flare, increase your fluid intake to prevent dehydration from diarrhea. You may need to modify your diet temporarily, typically by reducing fiber and avoiding known trigger foods. Keep track of your symptoms, including frequency, severity, and any associated factors – this information helps your healthcare team adjust your treatment plan.
For medication side effects, know which warning signs require immediate attention: high fever, severe abdominal pain, significant bleeding, or signs of allergic reaction like rash, swelling, or difficulty breathing. For these serious concerns, don’t hesitate to seek emergency care.
For less urgent side effects, contact your provider before stopping any medication. Sometimes simple adjustments like taking medications with food or at different times of day can help manage side effects while maintaining the benefits of treatment.
“I encourage patients to report significant adverse events to FDA MedWatch,” adds pharmacist Robert Chen. “This reporting helps identify patterns and improves medication safety for everyone.”
Cost, Insurance & New Drugs on the Horizon
The financial reality of colitis medication can be as challenging as the physical symptoms. Biologic therapies often cost between $30,000 and $50,000 annually without insurance coverage. Even the newer small molecule drugs come with similar price tags. Perhaps surprisingly, even older medications like 5-ASAs can be quite expensive.
“The cost nearly made me give up,” admits Janelle, who was prescribed a biologic after other treatments failed. “But my doctor connected me with a patient assistance program that made it affordable.”
Most pharmaceutical companies offer patient assistance programs for those who qualify based on financial need. These programs can significantly reduce or even eliminate out-of-pocket costs. Additionally, many manufacturers provide copay cards or savings programs for commercially insured patients, sometimes bringing costs down to as little as $5 per month.
When dealing with insurance, persistence often pays off. If coverage is denied, work with your healthcare team to appeal the decision. Having your doctor document why a specific medication is medically necessary can make all the difference. During insurance open enrollment periods, carefully review formularies to see which colitis medications are covered at the lowest cost tier.
Generic medications and biosimilars can offer significant savings. Generic versions of 5-ASAs like mesalamine can cost substantially less than brand-name versions. Biosimilars – which are highly similar versions of original biologic drugs – typically come with price tags 15-30% lower than the reference products.
Looking toward the future, the pipeline of new colitis treatments offers hope for better options. New IL-23 inhibitors are showing promising results with potentially better safety profiles than current biologics. Gut-selective JAK inhibitors aim to provide the benefits of current JAK inhibitors with fewer systemic side effects. Perhaps most exciting are emerging microbiome-based therapies that target the gut bacteria imbalances associated with IBD.
Clinical trials offer another avenue worth exploring – not only for potential access to cutting-edge treatments but sometimes also for free medication and monitoring during the study period. Your gastroenterologist can help determine if any available trials might be appropriate for your situation.
At Gladiator Therapeutics, we’re committed to developing innovative approaches that complement traditional medications. Our SemiCera® Technology represents our contribution to advancing treatment options for inflammatory conditions like colitis, with a focus on improving outcomes while potentially reducing long-term treatment costs.
Frequently Asked Questions about Colitis Medication
How long will I need to stay on colitis medication?
When patients ask me this question in my practice, I often see the concern in their eyes. It’s natural to wonder about the long-term commitment to colitis medication. The truth is, there’s no one-size-fits-all answer.
For most people with ulcerative colitis or Crohn’s disease, these are lifelong conditions that require ongoing management. Think of it like managing diabetes or high blood pressure—conditions we control rather than cure. Microscopic colitis sometimes follows a different path, occasionally resolving completely with treatment.
The duration of your medication journey depends on several personal factors. If your disease affects a larger portion of your colon or is more severe, you’ll likely need longer-term medication. Those lucky enough to achieve deep remission—where both symptoms disappear and the intestinal lining heals—might have more flexibility, but even then, caution is key.
I’ve seen many patients who feel better and stop their medications, only to experience a flare within months. As Dr. Jennifer Smith, an IBD specialist I’ve worked with, often says: “We’ve learned that stopping medications when patients feel better often leads to relapse within 6-12 months. The current approach aims for sustained control of inflammation to prevent both symptoms and long-term complications.”
For mild, limited disease that stays in remission for extended periods, your doctor might discuss tapering or discontinuing some medications. But this is a carefully monitored process, never a cold-turkey decision you should make on your own.
Can I safely combine different colitis medications?
“Is it safe to take all these medications together?” This question comes up in almost every consultation I have with newly diagnosed patients. The good news is that combination therapy isn’t just safe in most cases—it’s often the most effective approach.
Think of colitis medication combinations like a team where each member has a specific role. For mild to moderate ulcerative colitis, using both oral and rectal 5-ASAs can work better than either alone—one works from the top down, the other from the bottom up. For more severe disease, adding an immunomodulator to a biologic not only increases effectiveness but helps prevent your body from developing antibodies against the biologic.
I remember one patient who was hesitant about taking multiple medications until I explained it this way: “If you were trying to put out a large fire, would you use just water, or would you want water, foam, and other firefighting tools?” As Dr. David Chen, a pharmacologist I respect, puts it: “Combination therapy is like using multiple tools to fix a complex problem. Each medication addresses inflammation through different mechanisms, potentially providing synergistic benefits.”
Of course, more medications mean more things to monitor. Your healthcare team will watch for increased infection risk, potential drug interactions, and additional side effects. The benefits of better disease control often outweigh these concerns, but it’s a balanced decision you’ll make together with your doctor.
Are there natural approaches that replace prescription colitis medication?
I hear this question frequently, especially from newly diagnosed patients hoping to avoid pharmaceuticals. While the desire to take a natural approach is completely understandable, I need to be straightforward about what the evidence shows.
Currently, natural approaches work best as complements to conventional colitis medication rather than replacements. Some probiotics, particularly the high-potency formulation VSL#3/Visbiome, have shown benefits for mild ulcerative colitis and pouchitis. Curcumin (from turmeric) has demonstrated promise in some studies for maintaining remission, though we still face challenges with standardization and getting enough into the bloodstream.
Omega-3 fatty acids from fish oil show mixed results—helpful for some patients but not consistently effective across studies. Certain herbal therapies like boswellia and aloe vera have modest anti-inflammatory effects in small studies, but we need more research.
For children with Crohn’s disease, exclusive enteral nutrition—a specific liquid formula diet—can be remarkably effective, though it’s challenging to maintain long-term.
At Gladiator Therapeutics, we’re exploring innovative approaches using far infrared technology that may complement traditional treatments by promoting healing and reducing inflammation naturally.
Dr. Michael Brown, an integrative gastroenterologist colleague, offers wise counsel: “While complementary approaches can be valuable additions to conventional therapy, completely replacing proven medications with alternative treatments carries significant risks of undertreating inflammation, which can lead to complications and disease progression.”
The most balanced approach combines conventional medications with evidence-based complementary therapies, always with your healthcare provider’s knowledge. This integrated strategy often provides the best outcomes, addressing both the disease and your overall wellbeing.
Conclusion
Managing colitis is so much more than just taking pills and injections. It’s a journey that brings together medications, lifestyle changes, and a whole-person approach to health. While colitis medication remains at the heart of effective treatment, we’ve explored how your diet choices, stress management techniques, quality sleep, and regular exercise all work together to help you feel better and stay better.
The world of colitis treatment has come so far in recent years. From the trusty aminosalicylates that have helped patients for decades to the newest biologics and small molecules that target inflammation with laser-like precision, today’s options offer real hope. Many people who might have faced surgery in the past can now maintain remission with the right medication approach.
Your success in managing colitis comes through teamwork. It’s the partnership between you and your healthcare providers. It’s the collaboration between different treatment approaches. It’s finding the right balance between your medications and the daily choices you make about food, activity, and stress management.
At Gladiator Therapeutics, we believe in this holistic vision of healing. Our innovative SemiCera® Technology represents our commitment to exploring new approaches that might complement traditional treatments. We’re excited about contributing to a future where inflammatory conditions like colitis can be managed even more effectively, with fewer side effects and better quality of life.
Finding your path to remission might take some twists and turns. The medication that works wonderfully for someone else might not be right for you. The diet that triggers one person’s symptoms might be perfectly fine for your system. This is why personalized care is so important, and why the relationship with your healthcare team matters so much.
With patience, persistence, and the right support, most people with colitis can achieve good control of their condition. You can look forward to days when your condition doesn’t dictate your plans, when you’re not constantly thinking about bathroom locations, and when you have the energy to do the things you love.
For more information about innovative products that might complement your current treatment approach, visit our products page.
This guide is meant to inform and empower you, not replace the guidance of your healthcare team. Always consult with your medical providers before making changes to your treatment plan, and report concerning symptoms promptly. Your journey with colitis is uniquely yours, but you don’t have to walk it alone.
- Tags:
- abdominal pain